Healthcare Workers & Burnout

No one would argue that the COVID-19 pandemic took the greatest toll on people working in the healthcare industry. It drained them mentally and physically working long hours and putting themselves and their families at risk. Their lives were put on hold and in many cases changed forever. When the pandemic first hit, healthcare professionals were lauded for their heroism—putting themselves and their families at risk to take care of patients with COVID-19. And, while they stepped up to meet the grueling demands, most report burnout, physical and mental health struggles, and some are leaving the profession altogether.
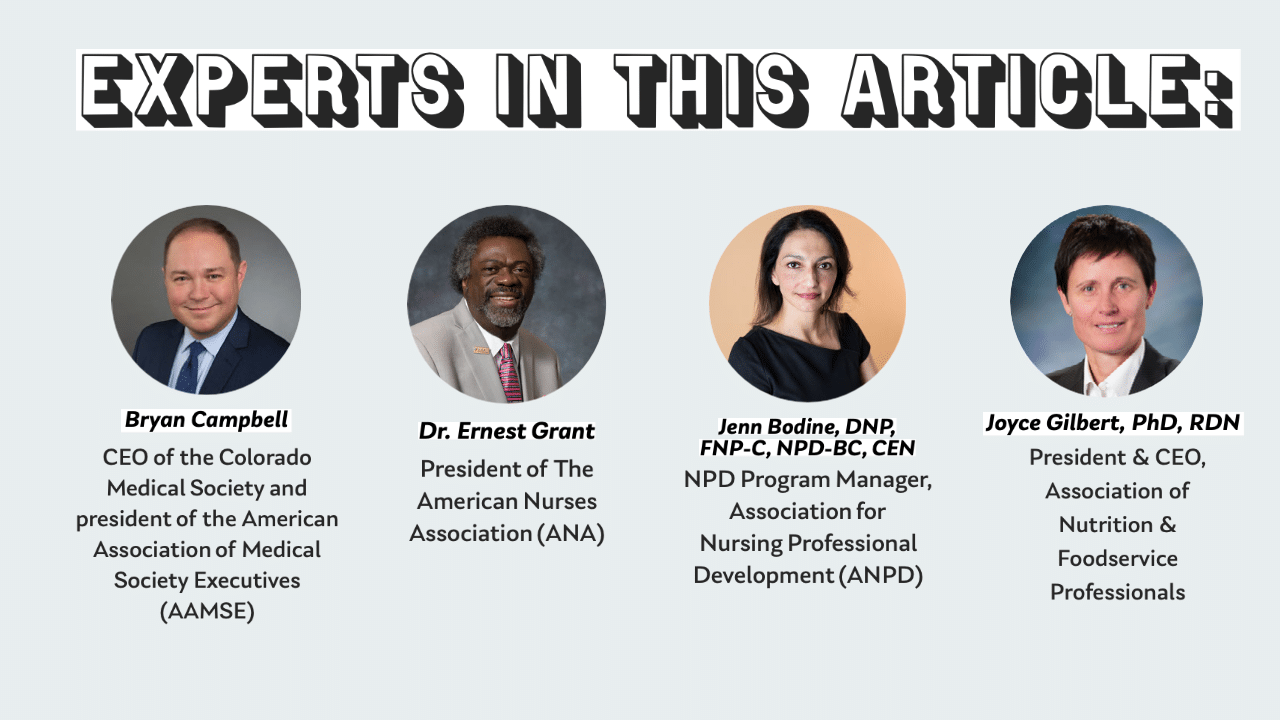
“The shine has worn off – at first people were shouting and cheering for healthcare workers; now they are shouting about being forced to take a vaccination. It’s 18 months of never-ending stress and now we are seeing an uptick in cases,” said Bryan Campbell, CEO of the Colorado Medical Society and president of the American Association of Medical Society Executives (AAMSE).
Developing the Right Resources
The American Nurses Association (ANA) surveyed its members to determine their needs and then quickly developed resources and mechanisms to help their members with burnout and stress. According to ANA President Dr. Ernest Grant, the biggest impact is the physical and mental fatigue that nurses continue to face from working a lot of overtime. Each time they return to work, they haven’t received enough down time, which increases the potential for errors in the workplace.
ANA collaborated with other nursing organizations to create the Wellbeing Project, which addresses the mental health needs of nurses. It includes resources and apps to support mental health and resilience. Among the resources is a self-assessment which helps members determine their stress level and needs. On resource is called the Happy App, and includes a 24/7 hotline for nurses to have confidential discussion about self-care and wellness. It also includes a narrative writing journal, a Moodfit App to track sleep, nutrition, exercise and more, videos, and a Nursing State of Mind podcast with episodes covering topics including:
- Who is on Your Team
- Balancing Work, Life, and COVID-19
- Hope is an Action Word
- Who Has Time for Self-Care
- Watching Your Emotional Signals
- Reconnect with Your Passion for Nursing
“We promoted the resources heavily to nurses and let them know there is no shame in seeking mental health assistance,” said Dr. Grant.
According to Jenn Bodine, DNP, FNP-C, NPD-BC, CEN, NPD Program Manager, Association for Nursing Professional Development (ANPD), their members were pulled from their primary NPD positions and back to the bedside to care for patients while also trying to deliver the education needed to keep the frontline informed of current best practices with regards to COVID-19 (which continue to evolve).
In addition, the NPD departments had to quickly orient nurses from one specialty to another to help cover staffing shortages in acute areas of care. This included new graduate nurses, many were unable to get the normal clinical rotations for their academic preparation due to the pandemic. They were introduced to a chaotic healthcare environment created by the pandemic.
“ANPD not only wants to support our members in their efforts to reduce their stress and burnout, but we also want to give our members resources that will help them to support frontline staff in reducing their stress and burnout. We helped our members by conducting, summarizing, and providing environmental scanning and just-in-time resources so that NPD practitioners could spend their time focusing on organizational needs,” said Bodine. Among the resources specifically geared toward preventing burnout and stress were NPD Café: Rise and Grind—Finding Flow in Work-Life Harmony, webinars, vlogs, and podcasts. They included a number of sessions specifically addressing these needs at the 2021 virtual convention including “Bend But Don’t Break: The Role of NPD Practitioners in a Global Pandemic.”
Beyond Resources: Advocating for Policy Changes
 Developing resources wasn’t the only way associations supported their members, many increased advocacy efforts as well.
Developing resources wasn’t the only way associations supported their members, many increased advocacy efforts as well.
“When COVID-19 hit, we immediately started to think about the impact of the pandemic on our members. We partnered with the Colorado Physician Health Program (CPHP) to set up a hotline for physicians who were struggling with mental health issues,” said Campbell.
However, in an unexpected turn of events, the Colorado regulatory agency made an announcement that it was awarding the CPHP contract to another company that would not guarantee confidentiality to physicians.
In response, the Colorado Medical Association partnered with the CPHP and stepped-up advocacy efforts, generating more than 2,000 letters from physicians to the Governor and other legislators demanding the CPHP be reinstituted. As a result, CPHP was reinstituted and physicians can once again access mental health services confidentially.
Beyond Burnout: Addressing Fleeing Healthcare Workers
 While healthcare workers got the most attention, non-healthcare professionals who work in the industry also felt the toll. The Association of Nutrition & Foodservice Professionals (ANFP) represents 15,000 members include certified dietary managers in acute care facilities, assisted living facilities, long term care and rehab facilities. These professionals oversee food service and are responsible for hiring cooks, aides and others in their departments.
While healthcare workers got the most attention, non-healthcare professionals who work in the industry also felt the toll. The Association of Nutrition & Foodservice Professionals (ANFP) represents 15,000 members include certified dietary managers in acute care facilities, assisted living facilities, long term care and rehab facilities. These professionals oversee food service and are responsible for hiring cooks, aides and others in their departments.
“The hardest part for healthcare and our members is the impact on labor due to so many people leaving because of burnout. As a result, our members who are certified dietary managers are taking on more responsibility and increased hours, but not getting paid for it,” said Joyce Gilbert, PhD, RDN, President & CEO, Association of Nutrition & Foodservice Professionals.
The ANFP establish a community where members could post and share their experiences and feelings. They also hosted a live conference in June. “We stacked the agenda with mental health topics and tied into our DEI initiative. We not only looked at what members needed but their employees too and built tools around how to identify burnout and isolation,” she added.
For the ANPD, the single biggest issue its members face now is figuring out how to navigate the experience complexity gap and the current nursing shortage, according to Bodine.
“As the baby boomer workforce retires in mass quantities, they take their years of experience with them, meaning we need to rely on the influx of novice new graduate nurses to backfill vacant positions. This situation has left healthcare with novice nurses who lack the experience to take care of the complex patient population who are living longer but not healthier. This phenomenon was expected to occur by 2030, however, the pandemic has caused this to happen ten years earlier and [nurses are leaving the profession]. This leaves NPD practitioners to figure out how to more efficiently and effectively train new hires and how they can contribute to the retention efforts of trying to keep existing nurses,“ she added.
“The greatest fear is going back to March of 2020 when everyone is on lockdown. Nurses on the front lines have not had any rest or enough downtime. As a result healthcare will implode upon itself and it’s the consumer who will suffer,” said Dr. Grant. “The care that they are expecting to get won’t be there.”
Want more articles relating to healthcare associations? View everything #healthcare here.
Tags
Related Articles
BAE Chicagoland Kicks Off: Join the Movement!
Black Association Executives (BAE) is officially in Chicagoland, bringing a bold new community to Black...
The Weight We Carry: What Teams Wish Leaders Understood
Association professionals are feeling the strain of relentless change—burnout, shifting expectations, and emotional fatigue are...
Workforce to Hit 30% Gen Z by 2030: Ready or Not?
Gen Z isn’t lazy—they’re reshaping work with speed, collaboration, and purpose. Here’s how to engage...





